Each Breath We take Trivia Quiz
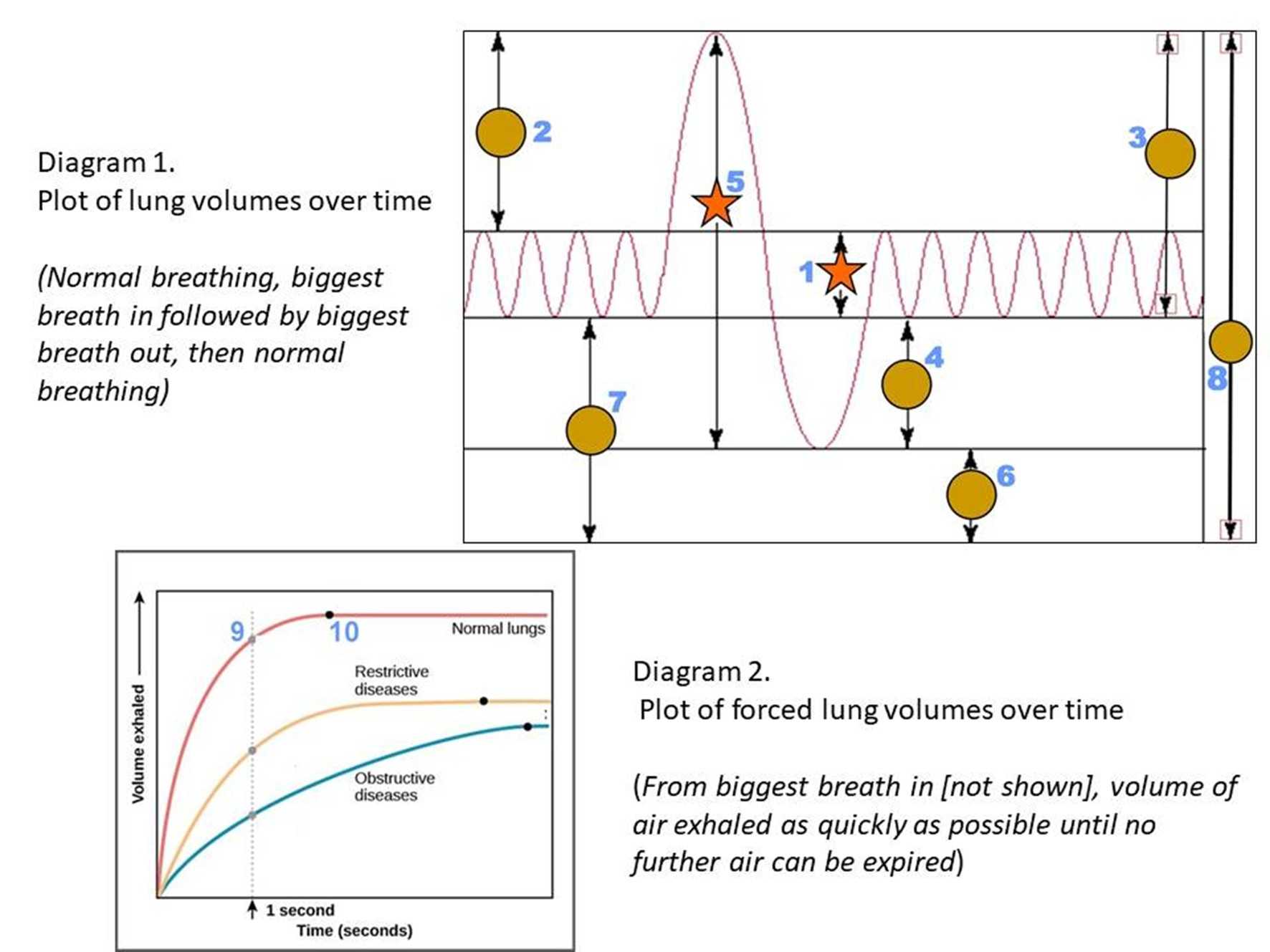
Lung Volumes in Health and Disease
The amount of air we breathe with each breath is a small percentage of the air in our lungs. There are various parameters with the volume of air in the lungs that changes in both health and disease. Let's explore these different respiratory parameters.
A label quiz
by 1nn1.
Estimated time: 3 mins.